“The human ego prefers anything, just about anything, to falling, or changing, or dying. The ego is that part of you that loves the status quo – even when it's not working. It attaches to past and present and fears the future.” ― Richard Rohr, Falling Upward: A Spirituality for the Two Halves of Life
The day before the Labor Day holiday was September 4, 2016, and it was a beautiful hot Sunday afternoon in Michigan. My wife, Michele, and I had arrived at a local winery on the water to meet friends and listen to one of our favorite musicians, Jim, who was also a friend. We had settled into our seats with a glass of wine and cheese and crackers.
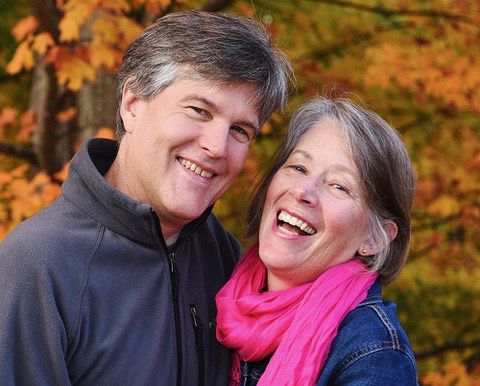
Jim started playing the Beatles’ “Here Comes the Sun,” and Michele said she’d like to dance. While Michele has a chronic autoimmune illness, some days are better than others. On this day, she felt pretty good. She has been a talented dance Hula-Hooper most of her life, so I fetched her hoop from the car, and she went off to the side so as not to bother others. About halfway through the song, I looked at her and thought, “Wow, she is beautiful and so talented.” I then returned my attention to Jim, appreciating his talents too.
When I looked back at Michele, she was no longer standing but lying - no - collapsed on the ground with the hoop still around her, lying backward. I stared for what seemed like an eternity, trying to figure out if she was taking a break or had fallen or something else. But, in reality, it was only seconds before I leaped up and ran to her. To me, she was convulsing and looked to be having a seizure. But I now know she was having a sudden cardiac arrest.
CPR
What a cardiac arrest “looks like” was unexpected, my wife vomited yet moved very little. She held my gaze for a long time as tears trickled down the sides of her face, an image that still haunts me today. Then her eyes closed and opened every now and then before shutting for—I feared—forever. When I got to her side, still thinking it was a seizure, I didn’t know what to do. I tried calling 911 on my cell phone but there was no reception. Luckily, the winery owner, Dave, walked by and asked, “Is everything all right? Can I help?” I recall yelling, “Please call 911—something has happened to my wife!”
Dave ran inside, trying his cell phone on the way, also to no avail. His landline got through. Then, he yelled, “Is there a doctor or nurse here? We have a collapsed woman on the lawn!” Amanda and Lance, a husband and wife from out of town, looked at each other. They had been wine-tasting all afternoon and didn’t feel quite sober, but Amanda had worked as an ER nurse for many years. Lance put his hand to her back, gently pushed forward yelling, “My wife is an ER nurse.”
Next, she was by my side directing, “We have to start CPR,” and started compressions. I then helped, and a third person helped as well. A couple of times, we gently rolled Michele to her side to clear away the vomit with our fingers and a towel. Although I now know that giving breaths is no longer a recommended step in the first response to a cardiac arrest, I did give her two to three out of desperation. After taking a CPR class since, I learned that compressions are the key—do not take up precious time with breaths.
We rotated compressions for about 15 to 20 minutes until the ambulance arrived. I have been told that CPR cannot be emphasized enough. At this critical stage, compressions have the best chance of saving a life. It’s the only way to keep the blood, or oxygen, circulating within the body. But it’s exhausting to administer compressions 100 times a minute to the tune, “Stayin' Alive,” for 15 to 20 minutes. If bystanders can help, it can make all the difference, as it did in our case. Shockingly, according to ER nurse Amanda, Michele’s heart stopped six times, then started again shortly afterward each time.
The emergency response team had their own heroics and anecdotes. One responder, Chris, happened to get the call when he was in a boat on the water just offshore from the winery. Because every second matters, the boat helmsman bypassed the dock and pushed the craft up on the lawn as an unknowing patron yelled, “You can’t park your boat here!” As EMT Chris leaped onto the lawn, running toward my wife 75 yards away, the skipper yelled back, “Today we can—he’s here to save a life.”
Other responders arrived and affixed an automated CPR machine to my wife. It was amazing to see it perform automated compressions and guide the response team on when to use the defibrillator. They had to use the paddles three times on Michele before her heart stabilized enough for transport.
Even though our hospital, Munson Medical Center, was only about a half-hour away, I was strongly encouraged NOT to drive myself to the hospital which was wise; I, or likely anyone for that matter, was in no state to drive. The ambulance team had me ride with them up front.
One darkly ironic event occurred on the way. Michele and I have had terrible personal experiences with motorcycles. Loved ones have been killed or hurt and we have had very negative experiences over the years from some drivers. Thus, I was stunned when we had to slow nearly to a crawl because we came up behind a large traveling motorcycle club who could not hear the sirens over the noise of their machines. It was a two-lane highway in peak traffic season for our popular tourist area. I thought, “If Michele dies because we did not arrive in time, I do not know if I will ever be able to live with myself.” They finally saw us in their mirrors and gave us room.
Hospital
The wonderful friends who met us that day at the winery then met and stayed with me at the hospital until Michele was stabilized, helping me retrieve my car later. One of them—Jim, the musician—bowed out of his concert performance and tore out right after we departed. He—and Penny, Pam, Doc, Donna, and Annie—helped me keep it together that evening.
I was sent home around 8 pm with the understanding that I would return first thing the next day with the usual list of items needed for hospitalized patients. I immediately jumped into the most pressing tasks, using them to burn off anxious energy. I took care of the cat, showered, and packed a small bag in prep for the hospital the following day. I called and updated Michele’s brother, my sister, then my brother. I then emailed my boss and coworkers, knowing they likely would not get the message until Tuesday after the Monday holiday.
The adrenaline was waning, and exhaustion was beginning to set in when I got a call from the hospital around 11:15 pm. The woman on the line, with the most foreboding words I have ever heard, said, “We need you to come to the hospital right away to discuss medical decisions for your wife. How quickly can you get here?”
Almost collapsing I held steady and replied, “I should be there in about 20 minutes.” I threw on the clothes I had ready, grabbed the prepped hospital bag and jumped in the car. Expecting the worst, I was not prepared for what I was told when I arrived. Attending cardiologist Dr. Anthony Ochoa said, “We need you to get in your car and drive to Grand Rapids right now.” Grand Rapids was about 2.5 hours away and had been a remote option when I left the hospital the first time, a few hours prior.
Dr. Ochoa explained that Michele could no longer be helped by the local hospital because it did not have the scarce medical technology called “ECMO” (extra-corporeal membranous oxygenation). To make a complex subject as simple as I can, it would serve as an external mechanical heart and lung for Michele. She would be in a medically induced coma, while her body healed itself with help from the ECMO support team.
ECMO equipment and trained-dedicated medical staff to run it is extensive and expensive, and the closest was Spectrum Health Hospital in Grand Rapids, MI. A medical transport plane was already on its way from Grand Rapids to pick up my wife. I needed to start driving immediately so that I could arrive at about the same time.
I was shell-shocked as I walked through the halls, making my way to the parking lot. I had to formulate a plan to head downstate, yet ensure someone could take care of our cat starting the very next morning, as well as other tasks. I called our friends, John and Michael, as I walked to my car. They lived near the hospital and my backup plan—if they did not answer the phone—was to drive to their home and pound on the door to awaken them to ask the favor.
To my relief, they picked up and offered their help immediately. I dropped off our house key to them on my way. Knowing our cat, Katie, would be in good hands, I had one less mental burden when I headed downstate.
Dr. Greg Marco, a pulmonary and critical care specialist at Spectrum Health in Grand Rapids, was wonderful, compassionate and unassuming. He met me around 4 am on Monday, Labor Day holiday. He had assessed my wife and was recommending ECMO and needed my approval. I said, “Thanks so much for explaining this, Dr. Marco. I am a data guy though. I need to know what we are up against. What are we talking about here? Can she make it? What are the odds; what are her chances?”
Dr. Marco, calmly explained, “In my experience, about 5% of the people who go on ECMO recover 100% or nearly 100%. They return to normal, healthy lives. About 70% of the people who go on ECMO do not make it all. Their situation is just too severe. The ones in between have some sort of challenge. By this I mean they may have some brain damage or, since circulation issues are common with ECMO, they may lose limbs or appendages because the external parts of the body may not get the nourishment they need.”
Then he paused and said, “I think your wife is a good candidate though.” I held onto that slim hope when I said, “OK, let’s do it.”
Coma
From Monday through Thursday that week, Michele was in a medically induced coma while undergoing ECMO treatment. There are many anecdotes and thoughts to share.
First, it is hard to understand what is going on with a loved one while they are in a coma. To my untrained mind, her condition changed from day to day, hour to hour or what seemed sometimes minute to minute. Looking back now, I chuckle when I facetiously say that she rarely responded to my voice—just like at home! Mercifully for my frail state of mind, I observed her respond consistently to the attending nurse or PA.
Early on I was told by the medical team, “She can hear you and us. She can smell and she will open her eyes on occasion and can see. Patients in a coma know to some extent what is happening around them. So please talk to her, squeeze her hand, touch her. Especially tell her repeatedly what happened and where she is. This can help reduce shock when we take her out of coma.”
Later that Monday I was taking a break and walking the halls of the hospital for the first of many long days. I was looking for dark chocolate. Michele and I are self-professed chocoholics. Especially Michele. Being a vegetarian for nearly 30 years at that point had possibly caused her to crave dark chocolate even more than expected - it was her only real vice. To make matters worse, we are dark chocolate snobs. Tongue in cheek, we have a problem and can be … arrogant about it.
By the time I inquired of the worker at the information counter, I was visibly distraught when she reminded me that because of the holiday many of the stores within the hospital were closed, as were most outside the hospital. I explained what I had hoped to do—get some dark chocolate and wave it under Michele’s nose. I wanted her to smell something other than the hospital room. Something familiar, something she would love. It was such a helpless feeling - I had latched onto this one thing I thought I could control, and it felt as if Michele’s life depended on my search.
Even now, as I remember the clerk’s response, I get choked up.
“Hold on,” she said and grabbed her purse, pulled out Hershey Dark chocolate squares, and gave them to me. “You need these more than me.”
I couldn’t speak. Sleep-deprived, terrified, and helpless, I accepted the chocolate and did my best to thank her through my tears. My snobbery gave way to gratitude over the humble Hershey bar.
A few minutes later, I waived the chocolate under Michele’s nose.
“I know this isn’t your brand of chocolate, honey, but it’s the best we can do now,” I said, adding the phrase I would repeat dozens of times over the days to come: “You had a cardiac arrest at the winery, and you are now in Grand Rapids at Spectrum Health Hospital.”
I don’t recall the exact day, but guess it was Wednesday when Michele’s mom visited being brought by Michele’s brother’s fiancé. She was 88 at the time; sometimes leaning on a walker, but most of the time denying she needed one. Sweet and caring as ever, she wondered how everyone else was doing, avidly asking if everyone was eating well.
I am still inspired by her strength and composure. Looking at her daughter in a coma she said through gentle tears, “It should be me in that bed. Not my youthful daughter.”
Our close friends Mike and Pam visited at one point bringing me a care package of my clothes and a gift. Pam had made a holy-healing stone. It was a rock mindfully found on our local beach with a hole in it into which was a wax-linen necklace. She instructed, “This is how you use it.” She rubbed it over Michele’s feet to pray for circulation to be healthy there. She then rubbed it on her hands saying, “May your creative, amazing talented hands be OK.” Then she rubbed it over her heart to help it heal and finished on her head so her mind would be intact.
It was wonderful to see and so touching. And, they also brought Michele’s brand of chocolate! From that point, I was able to wave HER chocolate under her nose many times a day. It felt as if I truly was helping her to heal.
While there had been some good progress, challenges and concerns arose every day. In one case on Thursday afternoon, I was asked to come to the room immediately.
The anesthesiologist in attendance held Michele’s very pale and bluish-looking hands and said, “We may have to amputate her fingers. We need to make some changes to the many IVs we have in her and hopefully, that will help, but we are very concerned about this.” After I explained that Michele also had Reynaud’s syndrome—a circulation problem that can make your fingers lose blood and look terrible—and perhaps that was the issue, the doctor replied, “Well, that is good to know and hopefully that’s it. This is still not good, though, and we need to make some IV changes.” The IVs were quite overwhelming - perhaps over a dozen were in her arms and hands. And my wife was always known as a small-veined person or a “hard-poke.”
But I was just shocked at the prospect of Michele losing her fingers. While I did not want her to die, of course, my wife was an award-winning artist, and her fingers were like life itself to her. Though her auto-immune disease severely limited what she could do, she was able to create some artwork over the years that was stunning. If she survived this only to wake up without fingers—I thought, she might have rather died.
I held myself as steady as possible and asked, “OK. While you do your next steps, can I do some things here too?” He said yes, of course.
I had remembered the holy-healing stone from Pam, and I had it with me. I went through the same thing Pam did—touching her feet, her heart, head and taking much time on her hands. I then left the room and walked around in a state of terror.
After 20 minutes I came back. The anesthesiologist was beaming. He showed me Michele’s hands, and they were pink and healthy and perfect. I about collapsed again, although this time from nothing but relief.
I think it was that Friday where the medical staff thought it was time. By this, they meant, as best they could tell, Michele had responded well to the ECMO treatment; her body had stabilized, and they wanted to remove the ECMO and bring her out of the coma. This is easier said than done.
Again, she had more than a dozen IVs connected to her arms, hands, and neck; and each made its own contribution to the overall life-saving suite of medications, such as kill pain, manage her vitals, keep her sedated, balance her blood chemistry, etc. They were going to remove the sedation first and then the others in turn, over a period, to gently bring her back to consciousness. I desperately hoped that would be the case.
Coming out of a coma is rarely an immediate event. It takes days and can be quite unnerving to watch. Your loved one often opens their eyes and shifts them across the room and closes them. They often slowly shake their head back and forth. Their limbs may jerk a little or move. This repeats on again, off again for days, depending upon the severity of the injuries and medication dosage. Michele had all of these.
Finally, Saturday night she seemed very awake and following everyone with her eyes but still had the ventilator—one of the last medical devices to be removed. Luckily, Michele (and pretty much all patients) was still very medicated at this state and did not appear to be in much discomfort. They asked me to leave the room while they attempted to remove the ventilator. After about 15 minutes they found me and explained they were not successful in that she was still struggling to breathe. They said that this is normal, and they would try again tomorrow.
I had gotten up early Sunday, had eaten and was walking coffee in hand down the long ICU hallway to Michele’s room when the doctor from the night before caught my arm. He said, “We got the ventilator out this morning! She is now wearing a positive pressure mask to force air down her lungs to help her breathe. This is normal and common for all patients like this. She will be hard to understand through the mask, but she is conversant!”
I was stunned and hurried to her room. I walked in and she was staring at me I think with somewhat of a smile, but the mask was quite large, loud and obtrusive. I sat down next to her and the first thing I heard her say was, “I almost died!” As tears ran down my face, I replied in full happiness mixed with a tad of sarcasm, “You’re right—you almost did!”
Then, I let myself believe she was going to be OK in the long haul when I heard her next words about our cat. “How is Katie?” Her priorities had not changed.
Communicate
The call I got Sunday night from the hospital was likely the worst call I have ever received. That was where I was asked to urgently rush back to discuss medical options. The worst call, then, that I have ever had to make myself was that next day on Monday morning. I had to call Michele’s dad. I can’t think of much that can prepare a husband to call his father-in-law and convey…that his only daughter died from a cardiac arrest the day before, was brought back to life, was now on a mechanical heart and lung and the odds were not looking good.
As I type I choke up yet again. I am too easily transported back to this moment when two grown people are on the phone, one trying to explain, the other trying to listen, while both are stuttering and halting through tears over the message. It took me a while to recover from just this one phone call.
Stepping back, no matter what, communication is a looming challenge in a situation like this. Not only who to update, but when and what. While I knew the first few days I would not be working, I expected—and was meditating on—that Michele would recover but it could take some time. I thought, perhaps, I would work from the hospital as much as I could in the days to come. Trying to work remotely, keep updated hourly on Michele’s medical status and keep myself “stable” was going to make it difficult for me to spend much time communicating.
This proved spot on, especially as her medical situation was volatile. Michele’s health would vacillate quite a bit throughout the day and then day-to-day thereafter. It was quickly confirmed that I could not, by myself, update tens of people every single day, yet somehow that needed to be done. I had a very long list of individuals who fell into these groups: Michele’s family, my family, coworkers, and friends.
I was lucky. I asked for and accepted offered help from family and friends. First, our friend Donna from the start volunteered to be my primary go-to person to “get the word out.”
The plan was for me to text her every day with any news. In turn, she would then send the message to key people who needed a regular update. One of these was my boss whose responsibility was then to pass on the information to my workplace. I had many coworkers and clients who needed to know, and he would help update them and field Q&A.
My brother was another recipient. He would then update my family and field questions from that group. Several others needed a current update as well, so they too were on a separate first-level list. I then called Michele’s brother, Kenny, each day.
This was incredibly helpful on many levels. One was that he could then update the rest of their family, which was a great help to me. Second, Michele is his only sibling, so he cared deeply about the situation and provided wonderful daily support to talk over her health for that day. Last, there were often some hard topics to discuss and some difficult information to digest and I desperately needed his help to navigate this. I remain deeply grateful to Kenny.
And I turned to social media. At first, I thought to myself, “I can’t put this on Facebook. This would just be tacky and would demean the situation.” As the first day after the event unfolded, however, other ideas came to my mind. I was fielding many calls, emails, text messages, and social media comments. I realized I needed to consolidate again. Perhaps I did need to post something in Facebook. After I sent out my first text-to-Donna update that night, I tried as sincerely and humbly as I could to share the same info on Facebook. It was one of the best decisions I made.
The outpouring of support, care and love was immediate, and I knew I had to continue. My eyes well up again upon remembering this experience. Prayer groups formed for us, many from family and others from people we didn’t know. (Thank you, cousin Cindy and Aunt Pat!) Every day, I received comments of love, support and encouragement. I didn’t realize how much I needed this.
Facebook post
7:15pm, 9/10/16: A very challenging day. The med staff explained the best approach is that of a marathon and not a sprint. Baby steps, some back, some forward. Until about 2 pm we weren't sure if she was going to come off the meds or if other issues were going on. They were talking about a CT scan to look for any new brain issues; i.e., stroke. Then, the PA came in a little after 2 pm and got Michele to respond to all questions and she moved every needed body part! After being frozen by the medically induced coma she was finally starting to thaw from the drugs wearing off. We could not remove the ventilator though--will try again tomorrow--and her heart is still weak. Again, it is day by day, often hour by hour. She is still in critical condition in cardio ICU and expected to remain there several more days. She knows me, is responding, making good eye contact but is really struggling to breathe. We have a long way to go and will do whatever we can to get there. Tnx for yr continued prayers.
We even learned that one of our friends was inspired to open a Facebook account to keep up on Michele’s progress. Many of us frown on social media for several good reasons, but it can have incredible utility and be a wonderful help. It made my life easier and better during Michele’s trials and proved to be an effective communication method.
The more specifics that I communicated about Michele’s health challenges; the more prayer groups had to work with. They consistently asked for details and would focus on helping Michele heal in these areas. I ended up posting on Facebook for many, many weeks, then gave monthly updates for a while.
For the second week of what we would be a total of three that I needed to spend at the hospital, I was offered a place to sleep at a young friend’s house close by. Michele and I were very close to his mother, and I was just blown away by his generous offer. I didn’t want to impose but now I am glad I took him up on it.
For the next week, I slept in a home instead of a hotel, and it felt very luxurious. When I got back each night, Josh already had dinner made. And I was greeted each evening by his four friendly, happy dogs—all rescued Pitbulls! I am an animal lover, and this was solace in and of itself. It was the constant human support, though—the amazing direct compassion each night—that was so comforting and helpful that week. We had some meaningful, touching conversations as well, and that was huge for my morale.
I can’t thank Josh enough. He is a wonderful person and I love him like a nephew.
Focus
“So whenever any kind of disaster strikes, or something goes seriously “wrong” — illness, disability, loss of home or fortune or of a socially defined identity, breakup of a close relationship, death or suffering of a loved one, or your own impending death — know that there is another side to it, that you are just one step away from something incredible: a complete alchemical transmutation of the base metal of pain and suffering into gold. That one step is called surrender.”
― Eckhart Tolle, The Power of Now: A Guide to Spiritual Enlightenment
After the first full day and night at the hospital, I woke up on a Tuesday morning. I was so fortunate that my sister, Julie, and brother-in-law, Chris, had stayed with me at the hospital and we went to breakfast. Despite their loving, giving presence, all I felt was pain. I felt like everything I saw, everything I experienced was through nothing but an elastic, many-feet thick layer of pain. That’s all I could … “see.”
That night I was trying to get back to sleep at 2 am—one of many instances of insomnia during this time. I deeply pondered how I was going to get through this. I then thought of every person I met so far, every individual with whom I interacted at the hospital and how wonderful they were in their roles.
The doctors, the PAs, the ECMO technicians, the nurses, the various therapists, the cleaning staff, the desk clerk. Everyone. Each expressed care at every moment, at every interaction. The volunteer who gave me a tour of the complex my first day there—a stranger—put her arm around me as she saw me struggle with composure while she navigated the campus on my behalf. The person at the information counter who shared her personal chocolate stash after listening to the story of my wife. The ECMO nurse who made a special point of washing my wife’s hair while she lay in coma. I will stop there, but this list goes on. Their care truly helped me in the most significant way.
I was struck by the exquisite match between their character and the roles they played. Then I asked myself a very hard question. What strength could I rely on to get me through “this”—whatever “this” was at the time and what “this” could be in the future? I knew I had to focus.
In my professional life, I was primarily a technical project manager. So, it came to me: I would treat this as a project, one that had one resource—me. I would give myself tasks each day to fulfill. It didn’t matter how big or trivial these were. Make two update calls to family today, check. Make three work calls from the hospital, check. Perform the online presentation from my hotel room that day, check. Study ECMO, with the help of the medical staff, and be able to explain it, check.
Throughout, I realized I naturally, semi-jokingly, herd people, and if I herded myself, like a project manager, I could survive. This is what, in the end, helped me stay “awake” and gave me some purpose each day. It didn’t matter about the pain layer of my being: I had tasks to do, and I simply needed to do them.
Help
“Failure and suffering are the great equalizers and levelers among humans. Success is just the opposite. Communities and commitment can form around suffering much more than around how wonderful or superior we are.”
― Richard Rohr, Falling Upward: A Spirituality for the Two Halves of Life
One thing surprised and humbled me. I learned to ask for and accept any and all help. In situations like these, it is not possible to do it alone. And so many people want to help.
From day one, John and Michael took care of our “child”—our cat, Katie—for three weeks driving 40 minutes out of their way twice a day. The day after the event—Labor Day— friends Vic and Georgia came by the hospital on their way home from an out-of-town trip. They not only gave much-needed support, but Vic lent me some of his unworn clothes to hold me over for a few days.
Many others came that day and on many other days that week. It was amazing support, and I am still grateful.
After a week or two, I received a check in the mail. It was from our friends’ church. We do not attend it, yet they chose to help us - and it was such a big help, emotionally and financially. The money covered my lodging and food for a week, and I felt less alone - yet another example of grace.
One time later, a coworker asked for our food preferences and brought in a food basket the next day. At another point, another friend emailed us with the same question. Two days later she showed up on our doorstep with tons of food. Another couple asked me to stop by their house on my way home from work. I picked up a care package basket of homemade food for several meals. It included chocolate!
During one of the evenings when Michele and I were “living” at the hospital for weeks, our mail carrier asked me via Facebook if she should hold our mail. She didn’t have to do this. We then learned that she would print out my daily Facebook posts each night and read them the next day on her mail route to our neighbors and friends who didn’t have Facebook. When Michele was finally home, our mail carrier came to our door to deliver a package. She walked into our living room and gave Michele the mail and a big hug!
Later we learned of a similar anecdote. Mary, a local business owner and friend, also printed out the evening Facebook updates to read to her coworkers the next day. When I came in for the first time since the event, I too was greeted with a hug!
Speaking of mail, while in the hospital, Michele received hundreds of get-well cards and packages. To the many inquiries from family and friends on how to help, I had sometimes answered that a card might help cheer up Michele, as I had no other suggestions for them. They sure responded! Michele loved every piece. One hospital volunteer who made the rounds most days commented, “I’ve been delivering mail here for almost 20 years, and I’ve never delivered so many cards to one room before!”
Also, my workplace was amazing. All my co-workers helped cover my tasks. Plus, the ongoing outpour of positive comments via Facebook, texts and emails simply made my day, every day. For the many weeks that I lived at the hospital, the support was such a relief.
Miracles
Since Michele’s cardiac “event,” I always say my wife is a walking miracle. She not only survived a cardiac arrest but also life-threatening blood clots that resulted from one of her in-coma medications. These both occurred simultaneously with her chronic autoimmune disease that she lives with every day.
In my mind, several minor miracles allowed her to be here today.
The first is that she was not alone when her SCA occurred. This is one reason only 1 out of 10 SCA victims survive: no one is there to help.
Second is that ER nurse Amanda was at the winery that fateful day and started expert CPR. This is the second reason that SCA victims do not make it: CPR, for whatever reason, is not performed, possibly because bystanders do not know it is needed or are not trained to do it.
Third is the miracle of medical technology in the form of ECMO. The person credited for developing this life-saving treatment modality is Dr. Robert Bartlett from the University of Michigan. Without ECMO, Michele would not be here.
Fourth, when Michele started having an allergic reaction to heparin, the default blood thinner for ECMO patients, the medical staff were able to diagnose and treat it fast enough to make a difference. When someone has heparin-induced thrombocytopenia or “HIT,” they develop blood clots, which can be life-threatening. This is ironic because this is the very health issue heparin is supposed to prevent.
Last, there were many people praying and meditating on our behalf. I was told this by countless people during and long after the event. I have many religious people in my life, mostly Christian and some Buddhists which is where my practice lies. I am not a spiritual expert and do not have the confidence to expound on how this helped in detail. But I believe it did.
Recovery
There is one intangible aspect to survival I need to state as it may not be obvious herein, but it permeates our lives. Michele and I have been known as a “silly” couple; we have very good and often irreverent senses of humor. It has been one of the key foundations of our relationship and we think it also one of the foundations of recovery. Humor can offer release and empowerment in a situation you may not control. I don’t think I can underscore this enough.
On a more tangible aspect, the medical staff told us, and we agreed, that a hospital is not a good place to rest or sleep. It is ironic that its biggest strength is also its biggest challenge. It can take care of patients 24/7 every day of the year regardless of weather or electrical power. They check on or perform diagnostics on every patient around the clock. From blood draws to weight checks to urine samples. The expert staff consists of nurses, doctors, occupational therapists, respiratory therapists, radiography technicians, and the list goes on. In their absolute defense, it is not possible to consolidate all care into one or two optimal visits for each patient. The workload is just too deep and broad.
It is only at home when a patient can really start to get rest, sleep and more effective healing. The sooner you can bring a patient home the better. Recovery will be faster.
Next, keep in mind that an event like this is very, very difficult for everyone involved. The amount of stress on the patient, the patient’s home caregiver(s), family and friends is extremely high. Michele had her own stress, trying to focus on recovery. In the end, she was a dutiful, positive, compliant patient, intensely focused on healing, following all medical instructions from medication to occupational therapy to diet. With great support, she has recovered wonderfully so far.
I am compelled to comment, however, on my experience as well. I was there from the start, where I ran to her side, helped with CPR, rode in the ambulance, drove downstate to an unknown hospital, lived at the hospital for three weeks, brought Michele home, helped with occupational therapy support, drove to follow up appointments, and many other tasks for many months. While I tried to do all these things, I also tried to hold down a full-time job as I am the primary income-earner for our household.
I found this incredibly stressful. My anxiety was at a life-time high. Some of it was caused from haunting imagery of Michele dying before me several times where I saw her tears run down her face as we held each other’s gaze. I was waking up in the middle of the night countless times to this nightmare, plus other related memories.
When I finally returned to work full-time, we had agreed we would text each other about once an hour. One instance—because life is simply this way—she hadn’t responded for many hours. I didn’t know what to do—I then called and left a voicemail. I waited a few minutes and - in a flood of worry - started to pack up my bag to rush home when I got her text. “So sorry! I had to take nap! Love you.”
Between my very stressful job and our intense experiences, I realized I was suffering with my own PTSD at some level. My doctor referred me to a therapist, and it was incredibly helpful.
Michele’s amazing recovery was also therapy and recovery for me too. But I also had my own and separate issues and challenges. I now realize the importance of investing in emotional help with someone trained to provide it. I found almost immediate relief. My only regret was that I did not pursue it earlier.
Celebrate
It is important to celebrate every improvement. To keep yourself in a healthy frame of mind, every small advance needs to be noted, as it is an antidote to the overwhelming loss and changes that have occurred. When Michele first stepped outside her room with Kevin, her encouraging physical therapist on 5 Heart, Spectrum Health Hospital, she was intimidated by the idea of walking around the hallway. She was weak and in the middle of what we would call a “brain fog” that lasted many weeks. The fog was from the coma, the medications, her body recovering itself—her total mind and body “reboot” as a friend described it.
But she took Kevin’s lead and made great progress that day. Later they navigated stairs, much to her astonishment. And after two-plus weeks she could finally take a shower on her own. This was huge and “felt so good,” she kept saying.
While in this state of recovery, it is hard to concentrate and to focus, and having visitors proved very difficult and taxing. Michele loved family and friends, of course, but found interacting with others exhausting at the time. This limited energy needed to be saved for the medical conversations and other tasks that occurred off and on throughout the day, sometimes at length.
Because of this, I was surprised once when I was on the phone in her room, changing personal appointments. We had been away from home for weeks, and I was trying to adjust calendars on the fly. She frantically waved at me and interrupted, saying she wanted to talk to the person on the other end. I took this as a very good sign - she was becoming interested in and able to handle even small interactions. Well, maybe not so small. I was talking to our hairstylist, and Michele was burning to know what to do about her hair after all of this. Yep, it is true that he was the first person she talked to over the phone since her SCA!
When home, we went through many other advances. Michele used a walker for a couple of weeks until it was safe to retire it. She used a shower chair for a time. She eventually took on laundry chores again, and we chuckle over a coworker’s comment, “I think I would have drawn that out.”
One day, we took our first walk in the woods. Michele held my arm as she was very unstable. I found a relatively flat and beautiful trail that we could walk for a quarter mile then turn around.
She did a half mile that day, at a slow, steady pace. We enjoyed the rejuvenation from nature and the return to a favorite pastime. It helped us both to restore resiliency.
A couple of months later, we visited the Spectrum Health Hospital for follow up visits. It’s surprising to realize that our ICU medical staff really don’t know—really can’t find out—what happens to patients who leave their care. It’s only by an active effort of the patient that they can get an update.
When we got to the 6 Heart floor of ICU, where Michele was on ECMO, we started a walking lap around the hall, me pushing Michele in a wheelchair since her stamina was still many months away from returning to normal. As we came across our admitting doctor, Dr. Marco, who implemented ECMO, the ECMO Nurse, Bina, and several others, they recognized us right away. There was nothing but tears in our eyes for me and the health staff. Michele did not grasp the significance at that moment—she didn’t know any of these people because she was in a coma the whole time under their care.
Then there was the dark chocolate. Recall we both have “problems” in that we are addicted and very snobby. Michele did not crave—did not even want—any chocolate in the immediate months following the event. It was just bizarre.
One of our wonderful PAs, Carrie, laughed with us at length on this. Carrie predicted and was right that one day Michele would eat chocolate again. A couple of months later, we were buying Christmas presents and Michele had bought some dark chocolate-covered cherries for gifts. She decided to take a bite. I jokingly said, “Watch it - that’s a gateway drug!” That January she started eating chocolate again daily.
We still had much to celebrate and to be thankful for. Luckily, our friend, Jim the musician, had the presence of mind to collect ER nurse Amanda’s contact information that fateful September day at the winery concert.
We organized a get-together that spring. Amanda, her husband, Lance, and many of our friends met up at another concert - at the same winery where Michele’s cardiac event occurred, with the same entertainer: Jim the musician. We agree with the wise adage: when you fall off a horse, get back on. It worked for us.
We have done many “celebration parties” since. They are wonderful for healing and recovery. One of the many touching celebratory moments was when, after 30 days in the hospital, I was finally bringing Michele home.
Facebook post
9pm, 9/30/26: I'll send another update again later but wanted to send one for today's milestone. Wow. Where to begin. First . . . Michele is . . . HOME. Yep. While waiting for the right delicate, medical balance for the ICD implant this week the PT's worked closely with her and she did GREAT! They said no need to go to a rehab facility because she already passed their care level and just needs in-home PT and nurse visits now. And, she got the ICD yesterday and passed overnight observation. And, they did another echocardiogram this week (#5?, lost track). It showed SIGNIFICANT improvement in her heart already. Wow. While the last month has been the worst of our lives, this day has been amazing and multi-faceted. Great news all around, she's home, much improvement . . . yet we r overwhelmed w the medical process going forward (medications, dozens of follow up visits, many more tests, etc.). And, she's/we're scared--scared it could happen again. We've been trying to get our arms around the odds (very slim) and the "insurance" of the ICD. It will take time. Related and despite her incredible progress, it will also take time for Michele to regain more strength, balance and stamina; something she'll be working on in the coming months. Everyone's positive energy, thoughts, prayers and support has been critical for helping us get through. THANK YOU! After a month in the hospital, driving home together was a rebirth. Michele raved at the views along the bay and winding roads, views we have seen thousands of times, yet r seen anew when given such a gift. And . . . she literally cried w joy . . . as we drove up our driveway, saw our house and pulled into our garage. Then we went in . . . to see her cat. ❤️
Thank people
Michele is walking today because of a plethora of reasons. If none of them would have been in place, this story would be different. To be accurate, there are many reasons that we’re aware of and, simply many that we are not. Who really knows how the universe works?
You can choose your belief, science, or rubric. Perhaps they all boil down to the same at their essence. Whatever that is, it has resonated with us. “We feel blessed” is our largest understatement since 9/4/2016.
The medical staff were amazing. The in-home healthcare she received was amazing. The “miracles” we experienced were, well, miracles. The support we received during and after has been heart-warming. From family, from coworkers, from my employer, from friends, from our community. We are astounded and exceedingly grateful.
Michele has written hundreds of cards; we have donated to various causes; we take each day as the gift that it is. When Michele discovered that ECMO inventor Dr. Bartlett was still in Michigan, she sent him a thank-you card and received a very touching note in return.
On one of my last days at Spectrum Health, I tried to put my experience into some perspective. I tried to thank the medical staff and to meditate on all who suffer.
Facebook post
5:30, 9/24/16: If Michele's positive trends continue, this will likely be my last post until we move her to rehab. I'm happy to say she's still making slow, but steady progress. She, me, and the med staff r in the home stretch to get her to this next phase--we all know how important this is as soon as her health is ready. There r still many steps though that r estimated to take 5-9 days. Since this will be my last post for a bit then, I hope u will allow me a moment to reflect. As I walked through the hospital halls for what was likely hundreds of times, it became quickly clear that ours is not the only traumatic story. Regardless of HIPPA you can't help but overhear or see others' challenges at a glance. Every room on the cardiac ICU floor has a traumatic story. As did every child without hair I passed in a wheelchair in the children's hospital. "Living" on the cardiac floors for three weeks, you hear many pages for code blue...some for adult, some for children and...one two rooms down from Michele. It is all humbling regardless of yr own pain. Yr prayers for us and the compassion of the entire Spectrum med staff for Michele's current challenges, and those for her heart in the coming months, r truly a blessing--we r blessed. I do hope these others r helped also. I know it may be pretentious to pray/meditate for all those who suffer and for those that help the suffering...but there is no harm in trying. Everyone "in our corner" has displayed boundless compassion and that, I think, is one of the finest expressions of grace. I sincerely thank you for yr example; it is an inspiration . . . to be a better person. ❤️
Last Comments
“It is not impermanence that makes us suffer. What makes us suffer is wanting things to be permanent when they are not.”
― Thích Nhất Hạnh
I am writing this several years after the incident. Some reading it may have been “there” at some point during the ordeal and may remember differently and more accurately. To this, I ask your forgiveness if I am off on some details.
For many reasons, I waited a while before writing about this experience. The main reason was that I needed space to process the event, emotionally and intellectually. After many requests, I was compelled to finally sit at the keyboard. I certainly hope it was helpful and of some interest.
I do not wish—ever—that you or anyone must go through a similar situation. If you find yourself in “it,” however, perhaps these words will have helped in even the smallest way.
Take a CPR class. Do this now, before you need it. Ask for and accept all help. Find good ways for you to communicate. Make sure you take care of yourself—healthy diet, sleep and professional mental health help. Focus on how to survive the event. Find humor wherever you can. Thank people—over and over. Celebrate in some way, big or small, every day.
By Andy LePere
