GRENOBLE, FRANCE--Gasping for air before or during CPR for out-of-hospital cardiac arrest (OHCA) is a strong predictor of survival with favorable brain function, new research suggests.[1]
Besides ventricular fibrillation (VF)/ventricular tachycardia (VT) as the presenting cardiac rhythm, spontaneous gasping before or during CPR appears to be a “major prognostic variable” in predicting 1-year survival with favorable brain function, the researchers report. They say the combination of these two natural biomarkers “provides the highest reported predictive markers of long-term survival with favorable brain function.”
The study was published in the September 19, 2017 issue of the Journal of the American College of Cardiology.
“This study is the first to report the importance of gasping as a predictor of long-term survival with favorable brain function after out-of-hospital cardiac arrest,” said first author Guillaume Debaty, MD (University Hospital of Grenoble, France). “Gasping is now the second predictive factor for good neurologic outcome. Regardless of the presenting cardiac rhythm, 37% of long-term survivors with favorable brain function had agonal respiration during cardiopulmonary resuscitation,” Debaty said.
“These findings underscore the importance of recognizing gasping during CPR and strongly support collecting data on gasping in all future out-of-hospital cardiac arrest trials and registries,” Debaty added. The findings also provide a potential rationale for not terminating chest compressions or inhibiting spontaneous inspiratory efforts in a gasping patient during CPR, the researchers say.
“Remarkable” Predictors
Gasping is a natural reflex that enhances oxygenation and circulation during CPR and is a natural biomarker for the presence of brainstem activity. However, a lack of knowledge about the importance of gasping during CPR may contribute to the lack of reporting, tracking, and attention to this natural biomarker in the setting of cardiac arrest, the researchers say.
To investigate the long-term prognostic value of gasping during OHCA, they did a secondary analysis of prospectively collected data on gasping during OHCA in 1888 patients from a multicenter randomized controlled trial of standard CPR vs active compression-decompression CPR. They had information on spontaneous gasping or breathing for 1880 patients, 1-year survival data for 1840, and Cerebral Performance Category (CPC) score at 1 year for 1827 patients.
Overall, 197 subjects (10%) had spontaneous gasping or agonal respirations before or during CPR.
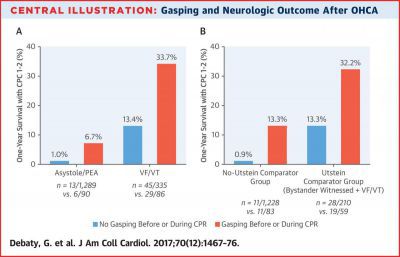
The overall rate of 1-year survival with favorable neurological function (CPC score of 2 or less) was 5.4% (98 of 1827). The rate was significantly higher in patients with than without spontaneous gasping during or before CPR (20% vs 3.7%).
In multivariable analysis, 1-year survival with favorable brain function was independently associated with gasping during CPR (odds ratio [OR] 3.94, 95% CI 2.09–7.44). A shockable initial recorded rhythm (VF/VT) was also an independent predictor of survival with good brain function (OR 16.50, 95% CI 7.40–36.81).
The combination of gasping and VF/VT as the first recorded rhythm was associated with a “remarkable” 57-fold higher likelihood of 1-year survival with good brain function (OR 57.0, 95% CI 23.49–136.92) compared with no gasping and no VF/VT, the researchers report.
Pulmonary edema was also independently associated with 1-year survival with favorable neurological function (OR 3.41, 95% CI 1.53–7.60). The underlying mechanisms for this association are likely multifactorial, they note.
Survival with good neurological function was less likely with younger age (OR 0.57 for each standard deviation, 95% CI 0.43–0.76), shorter CPR duration (OR 0.31, 95% CI 0.19–0.51) and lower prehospital epinephrine dose (OR 0.47, 95% CI 0.25–0.87).
In a recent meta-analysis with more than 10,700 participants[2], gasping was associated with an increased relative risk of survival to hospital discharge (OR 3.53, 95% CI 3.03–4.10).
“Our study extends this previous finding, with long-term survival with good brain function estimates being consistent in magnitude,” Debaty and colleagues write.
Immediate Clinical Implications
They note that gasping or agonal breathing can make it hard for bystanders to recognize cardiac arrest.
“Therefore, a special focus on whether a patient is gasping is recommended during CPR classes as well as for dispatchers during call-taking and the dispensing of pre-arrival instructions and dispatcher-assisted CPR,” they advise.
The authors of an editorial[3] published with the study say gasping following cardiac arrest is a natural biomarker “deserving attention.”
“The implications of their findings should be heeded,” write Gordon Ewy, MD (University of Arizona College of Medicine) and Paul Armstrong, MD (University of Alberta, Edmonton). “Recognizing that gasping is an early sign of cardiac arrest is of utmost importance.”
They also say this finding should be emphasized during CPR training, “so that bystanders do not misinterpret gasping as normal breathing. Recording gasping prospectively and systematically will inform future registries and much-needed research in OHCA.”
[1] [2] Zhao X, et al, Resuscitation, (97) 7-12 More...SOURCE: Megan Brooks, Medscape Medical News: Gasping Bodes Well for Survival After Cardiac Arrest - Medscape - Sep 13, 2017
