The perspectives of national key stakeholders during a National Institutes of Health funded workshop
According to new research published in Critical Care Explorations, acute brain injury from cardiac arrest and traumatic brain injury happens suddenly and unexpectedly, carrying high potential for lifelong disability with substantial prognostic uncertainty. Comprehensive assessments of family experiences and support needs after acute brain injury are lacking. To elicit “on-the-ground” perspectives about the experiences and needs of families of patients with acute brain injury, researchers conducted a two-phase qualitative study of families and multidisciplinary U.S. healthcare professionals with related expertise.
Members of the Sudden Cardiac Arrest Foundation survivor/caregiver network participated in this research.
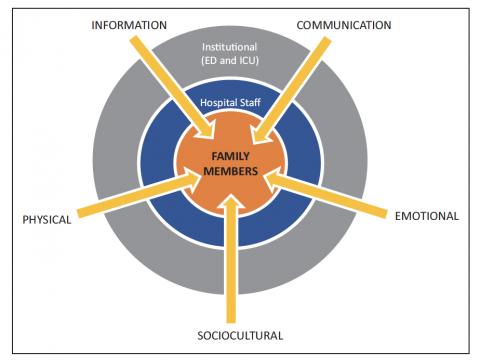
Participants identified four major needs:
- Challenges in coping with uncertainty in early prognostication
- Inattention to physical needs of family
- Deficits in compassionate and consistent communication
- Need for engagement with families as stakeholders in improving future practices.
As one family member said, “I was met at the door by a clergyman who took me into a little room which kind of scared me, because I knew that meant things were really bad, but it was a space that I could just be isolated from other places. And he stayed with me the whole time. And then there’s a whole compassionate care team at the hospital, and the first thing they did was give me this blanket that was knitted by Women in Prayer, which I cherish, and I’ve taken to the hospital any time he had to go back.”
Participants’ recommendations included:
- Ways to communicate more clearly and consistently
- Better assistance with navigating resources and access to places for families to care for themselves
- Opportunities for families to remain connected with their loved ones, social support networks, and the clinical team.
These factors can contribute to improved decision-making and physical/emotional outcomes. Interventions to address these unmet needs should be developed.
The research was led by Susanne Muehlschlegel, MD, MPH, Departments of Neurology, Anesthesiology/Critical Care & Surgery, University of Massachusetts Chan Medical School, Worcester, MA, and Sarah M. Perman, MD, MSCE, Department of Emergency Medicine, University of Colorado, Denver, CO.
