ROME, ITALY--Automatic external defibrillators (AEDs) fail to save lives when the public does not have basic life support education, according to research presented today at ESC Congress 2016. The study found that public access defibrillation (PAD) programs are unevenly deployed across France, with an obvious impact on out-of-hospital cardiac arrest (OHCA) survival rate.
“The survival rate of OHCA remains extremely low,” said Dr. Nicole Karam, an interventional cardiologist at the European Hospital Georges Pompidou in Paris, France, on behalf of the Paris Sudden Death Expertise Centre led by Professor Xavier Jouven.
“The importance of the early minutes of OHCA management is well recognized and PAD programs have been developed to increase both AED availability and basic life support awareness,” she continued. “However, no study has assessed the deployment of these programs in real life.”
The current study, coordinated by Dr. Eloi Marijon, was a five-year national prospective assessment of PAD programs conducted throughout 51 districts in France. The two arms of PAD programs were evaluated: density of deployed AEDs (per 100 000 inhabitants/1000 km2) and proportion of persons educated in basic life support at least once during the five year period (per 100,000 inhabitants), either by public governmental or private initiatives.
The researchers found huge discrepancies in PAD development across the districts. The proportion of educated persons varied from 6,955 to 36,636 per 100 000 inhabitants, while the density of AEDs varied from five to 3,399 per 100,000 inhabitants/1000 km2. Overall, only 35.3% of districts developed a significant program, defined by the authors as both AED density and educational rate above the median (more than 22 AEDs per 100,000 inhabitants/1000 km2 and more than 13,866 educated persons per 100,000 inhabitants).
“These discrepancies were way beyond those we expected,” said Dr. Karam. “Around a third of districts developed complete PAD programs, while others either did not invest sufficiently in any of the two arms (37.2%), or only focused on one of the two components. There was no correlation between the implementation rates of the two components, as if there was no global strategy to effectively deploy complete PAD programs.”
Another interesting finding was that there was absolutely no correlation between the level of national and local education, indicating a limited collaboration between these two decision makers. “We could have expected more local investment in districts with poor national investment and vice versa, but this is not the case, further highlighting the absence of real deployment strategies for PAD programs,” said Dr Karam.
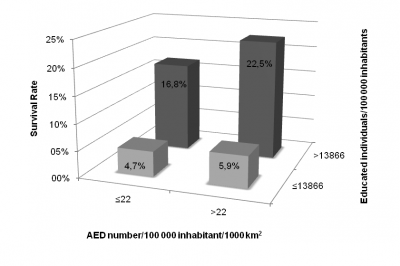
OHCA survival rate varied tremendously among districts, ranging from 0 to 43.8%. Survival rates increased with higher levels of PAD implementation, certifying their importance in improving OHCA outcomes. However, survival rates were low in districts with low levels of education, whether they had a high density of AEDs or not (5.9% and 4.7% respectively), and only increased with a rise in population education (figure 1).
Survival rate was much more correlated to the number of educated individuals (correlation coefficient 0.89) than to the number of available AEDs (0.25). In multivariate analysis, only the level of population education was independently associated with survival (odds ratio 1.64, P = 0.004).
Dr. Karam concluded: “Even though this study confirms the beneficial effect of PAD programs, it reveals a huge heterogeneity (more than 100-fold) in their implementation with an uneven investment in each of their arms. It also highlights the insufficient benefit of deploying AEDs if not combined with population education, which should be helpful in planning public health policies.”
SOURCE: European Society of Cardiology
