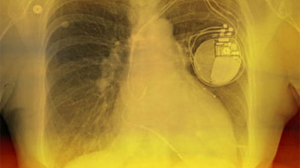
On Feb. 15, the Centers for Medicare and Medicaid Services (CMS) released a final policy decision updating the national coverage determination (NCD) governing implantable cardioverter-defibrillator (ICD) implantation for Medicare fee-for-service patients.
The NCD will continue to govern patient criteria and covered indications for CMS reimbursement of ICD implantation. In a notable change from the draft NCD released last November, the shared decision-making encounter does not need to be completed by an "independent" clinician. Instead, the final NCD specifies that the encounter involve a decision tool but does not require the encounter take place separately. This change comes in response to feedback provided by ACC President Mary Norine Walsh, MD, FACC, and George F. Van Hare, MD, FHRS, FACC, president of the Heart Rhythm Society (HRS), in a public comment letter after the draft NCD was released. In the comment letter, Walsh and Van Hare noted that shared decision-making "has long been an integral component of patient care in electrophysiology programs across the country" and that a separate formal encounter with an independent clinician "would be redundant to current workflow and could delay potentially lifesaving ICD treatment." ACC provides this type of shared decision-making tool on CardioSmart.org.
Among other specifics, the new NCD updates clinical indications and incorporates several exemptions for waiting periods. The NCD also ends the requirement for data collection for evidence development, which sites have satisfied through participation in ACC's ICD Registry. However, enrollment in the ICD Registry will continue to provide evidence of compliance with CMS reimbursement criteria. CMS noted in the NCD that the agency "encourage[s] the continuation and improvement of a voluntary registry for purposes of quality improvement, safety and appropriate use verification."
ACC and HRS in the public comment letter last fall recommended that the policy be updated to reflect current, evidence-based science and guideline recommendations that have changed since the policy was issued – including the 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death.
"Ongoing collaboration and coordination among CMS, the U.S. Food and Drug Administration, the National Institutes of Health, the Agency for Healthcare Research and Quality, and other federal agencies presents an opportunity to ensure funding and timely completion of well-designed studies to answer outstanding questions," Walsh and Van Hare wrote. "The Societies support the coverage with evidence development paradigm to expedite earlier access to innovative technologies that are likely to show benefit for the Medicare population where there is incomplete evidence."
The changes are effective immediately, though contractors must wait for further technical instructions from CMS before updating claims processing software. ACC staff are reviewing the final decision to identify any additional topics of interest to members.
SOURCE: American College of Cardiology
